Psoriasis: causes, symptoms, diagnosis and treatment.
Psoriasis is a chronic non-communicable disease that can affect various organs: skin, joints, heart, kidneys.
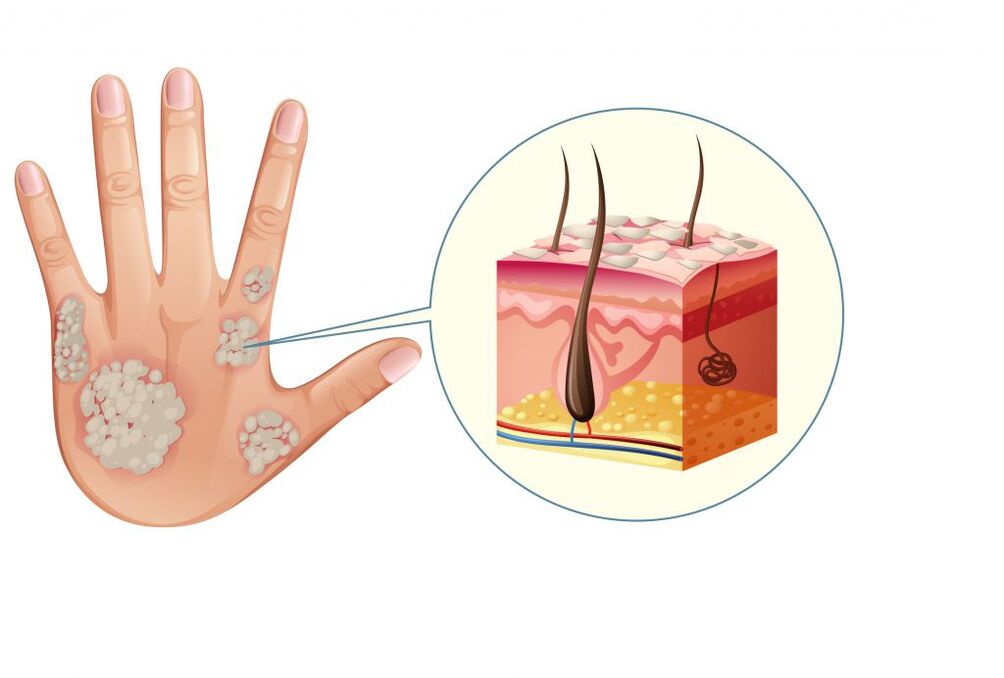
Most often, mild psoriasis appears on the skin as well-defined pink-red papules (nodules that rise above the surface of the skin), which merge into plaques with silvery-white scales.
In moderate and severe forms of the disease, the inflammatory process leads to damage to the musculoskeletal system and the cardiovascular system. Psoriasis has a relapsing course (relapse of symptoms after complete or partial recovery) and a tendency to cause comorbidities that compromise patients' quality of life.
Causes of psoriasis
The disease can be based on several triggers. However, it is not yet known exactly which of them are primary and which are secondary. Dysfunction of the immune system is considered to be the main cause that explains the onset of psoriasis. Cells aimed at destroying pathogens start attacking their own cells (mainly the skin). As a result, an inflammatory process develops, which causes accelerated cell division of the epidermis (epidermal hyperplasia) and the formation of psoriatic papules and plaques.
An inadequate immune response is often due to genetic characteristics.
Psoriasis is very often hereditary.
More than 40 chromosomal regions associated with the risk of developing psoriasis have now been identified. The onset of the disease can be caused by a weakening of the immune system against the background of stress, infectious and endocrine diseases. Psoriasis often accompanies allergic and immunodeficiency conditions, which are based on a violation of the immune response. Additionally, psoriasis can be triggered by certain medications (antidepressants, beta-blockers, non-steroidal anti-inflammatory drugs).
Psoriasis classification
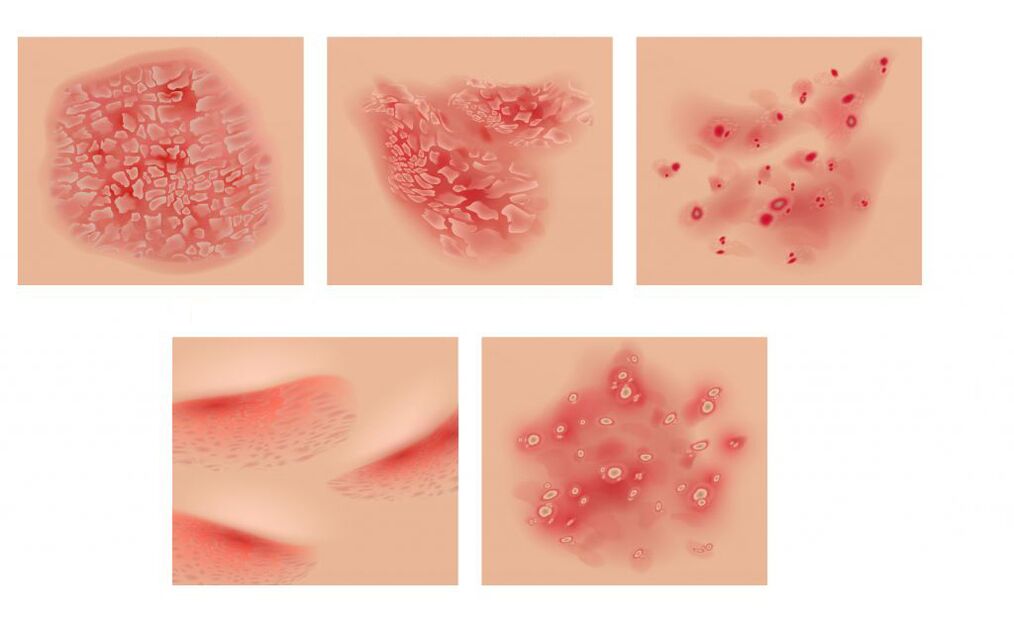
Depending on the localization of the pathological process, various types of psoriasis are distinguished. The most common is vulgar, orcommon, psoriasiswhen well-defined pink papules appear on the skin, which merge into plaques covered with white-silver scales. In case of damage to the scalp (seborrheic psoriasis) rashes in the form of yellowish scales can descend on the forehead, forming a seborrheic "crown". In patients with metabolic disorders, the plaques may show exudate, a fluid secreted during inflammatory processes (exudative psoriasis). In childhood and adolescence, especially after strep infections, the disease can become acute, with many bright red teardrop-shaped papules appearing on the skin with mild peeling and infiltration (guttate psoriasis). Sometimes there is pustular psoriasis, which is characterized by the appearance of pustules against the background of reddened skin, most often in the arch of the feet or palms.Psoriatic erythrodermacan occur against the background of exacerbation of ordinary psoriasis under the influence of provoking factors. Dry white scales cover the skin, it becomes bright red, swollen and hot to the touch. He runs very fastgeneralized Zumbusch psoriasis. It is characterized by the fact that small purulent vesicles appear on the reddened skin, which, merging, form "purulent lakes".Psoriatic arthritisaccompanied by damage to the joints and develops simultaneously with the rashes or precedes them.
Symptoms of psoriasis
The skin form of psoriasis is accompanied by the appearance of papules dotted with bright pink, sometimes in the form of droplets. Joining together, they form plates covered with silvery-white scales.
Rashes are found on the extensor surfaces of the arms and knee joints, on the scalp, on the lower back, and on the sacrum.
The upper layer of the plates is formed by easily removable scales of dead epidermis. Initially, they occupy the center of the plate, then fill the entire area. When the scales are removed, a bright bright red surface is revealed. Sometimes the plaque is surrounded by a pink border, a zone for further growth, while the surrounding skin does not change. The rash is accompanied by intense itching. With psoriatic erythroderma, patients develop fever (fever with chills) and severe itching against the background of rashes all over the skin and increased lymph nodes.
With a long course of the disease, hair and nails can fall out.
Generalized Zumbusch psoriasis is very difficult. Purulent rashes cover the entire skin and are accompanied by severe fever and intoxication. Psoriatic joint damage is characterized by pain and redness of the skin on the joint surfaces. Any movement is difficult, inflammation of the ligaments and tendons develops. With psoriasis, the nail plates are most often affected, while pinpoint depressions appear on the surface of the nail (a "thimble" symptom).
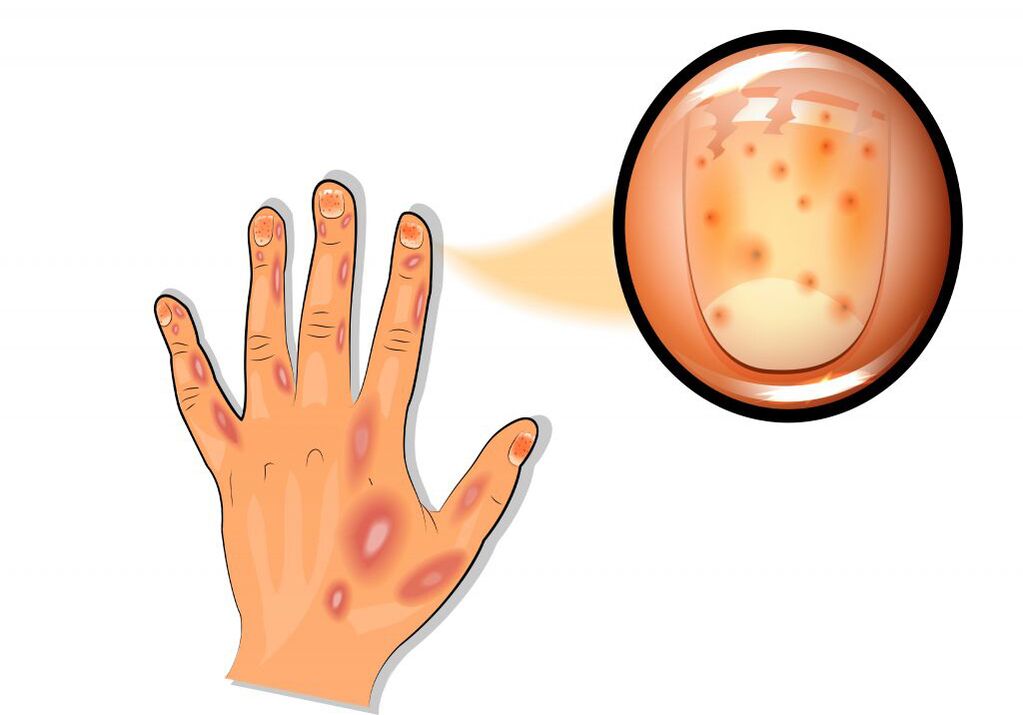
Small reddish and yellowish-brown spots appear under the nail plate at the base ("oil stain" symptom). Dystrophic changes often develop in the nails and hair.
In children, especially infants, the symptoms of psoriasis have their own specificities.
In the area of redness that occurs in the skin folds, effusion and slight peeling of the upper layer of the epidermis may occur. This image resembles diaper rash or candidiasis. Sometimes rashes appear on the skin of the face or in the genital area.
Psoriasis Diagnosis
It is possible to identify the disease on the basis of the symptoms of the psoriatic triad (stearic white surface of the papule; shiny reddish film after peeling off the scales and precise protrusion of the blood after its removal).
Another feature is the Koebner phenomenon. It lies in the fact that in the area of skin irritation, after 7-12 days, erythematous rashes appear (areas of redness and peeling in the area of scratches, scratches). Sometimes, to confirm the diagnosis, a histological examination of a biopsy of the affected skin area is performed. In addition, a clinical and laboratory examination is necessary: a clinical blood test, a biochemical blood test (total protein, protein fractions, C-reactive protein, ALT, AST, LDH, creatinine, electrolytes: potassium, sodium, chlorine, calcium ).
Which doctors to contact
If rashes appear, which often occur against the background of infectious diseases, skin lesions, stress, it is necessary to consult a therapist or dermatologist. In case of systemic damage to the patient's body, they can be referred to an ophthalmologist, endocrinologist, gynecologist or other specialists.
Treatment
Psoriasis affects both the skin and the musculoskeletal system, as well as internal organs. When rashes appear only on the skin, local preparations of glucocorticosteroids, ointments containing synthetic analogues of vitamin D3, activated zinc, salicylic acid and other components are recommended. Hormonal creams should be used with caution on skin prone to atrophy.
It is necessary to take into account the possibility of hormonal disorders with prolonged use of steroid creams.
The effectiveness of hormonal creams is increased in combination with salicylic acid, analogues of vitamin D. For the treatment of severe forms of psoriasis, second generation aromatic retinoids, based on acitretin, are used. The drug slows down the proliferation of epidermal cells, normalizes the keratinization process and has an immunomodulatory effect. Phototherapy (medium wave UV and PUVA therapy) in combination with retinoids is also recommended. As a systemic therapy, the doctor may prescribe immunosuppressive agents. If necessary, prescribe detoxifying and desensitizing therapy, plasmapheresis.
Complications of psoriasis
Psoriatic arthritis develops in 10% of patients, affecting the spine, joints of the arms and legs. Patients suffer from joint pain and morning stiffness. Features of psoriatic arthritis include the asymmetry of the places of its manifestation, which can be combined with damage to the nails. Psoriasis is often accompanied by concomitant or concomitant diseases.
Due to inflammatory vascular lesions, the risk of coronary heart disease and stroke increases.
It is also possible to develop diabetes and Crohn's disease. In some cases, the complications of psoriasis can lead to disability.
Psoriasis prevention
Measures to prevent psoriasis are mainly aimed at strengthening the immune system. Skin care should include hydration and nutrition. With a predisposition to allergies, it is necessary to control nutrition, avoiding fatty and spicy foods, excessive consumption of carbohydrates, potatoes. An obligatory component of psoriasis prevention should be vitamin therapy.
In addition, the functioning of the immune system largely depends on the state of the nervous system. People who are hyper-responsible, have a busy work schedule, and experience constant negative psycho-emotional impact are more prone to autoimmune diseases, including psoriasis. Therefore, the prevention of psoriasis, together with physical healing measures (giving up bad habits, physical activity), should also include the achievement of psycho-emotional comfort.
IMPORTANT!
The information in this section is not to be used for self-diagnosis or self-treatment. In case of pain or other exacerbation of the disease, only the attending physician should prescribe diagnostic tests. For proper diagnosis and treatment, you need to contact your doctor.
























